define quantitative futility as the judgment that a treatment has less than a 5% chance of achieving the desired physiologic result. Select one: True False
define quantitative futility as the judgment that a treatment has less than a 5% chance of achieving the desired physiologic result. Select one: True False
Biology: The Unity and Diversity of Life (MindTap Course List)
14th Edition
ISBN:9781305073951
Author:Cecie Starr, Ralph Taggart, Christine Evers, Lisa Starr
Publisher:Cecie Starr, Ralph Taggart, Christine Evers, Lisa Starr
Chapter37: Immunity
Section: Chapter Questions
Problem 3DAA: Cervical Cancer Incidence In HPV-Positive Women In 2003, Michelle Khan and her coworkers published...
Related questions
Question
Schneiderman, Jecker, and Jonsen define quantitative futility as the judgment that a treatment has less than a 5% chance of achieving the desired physiologic result.
Select one:
True
False
Transcribed Image Text:was not intended for them and they should not be
treated even if they were richer than Midas.
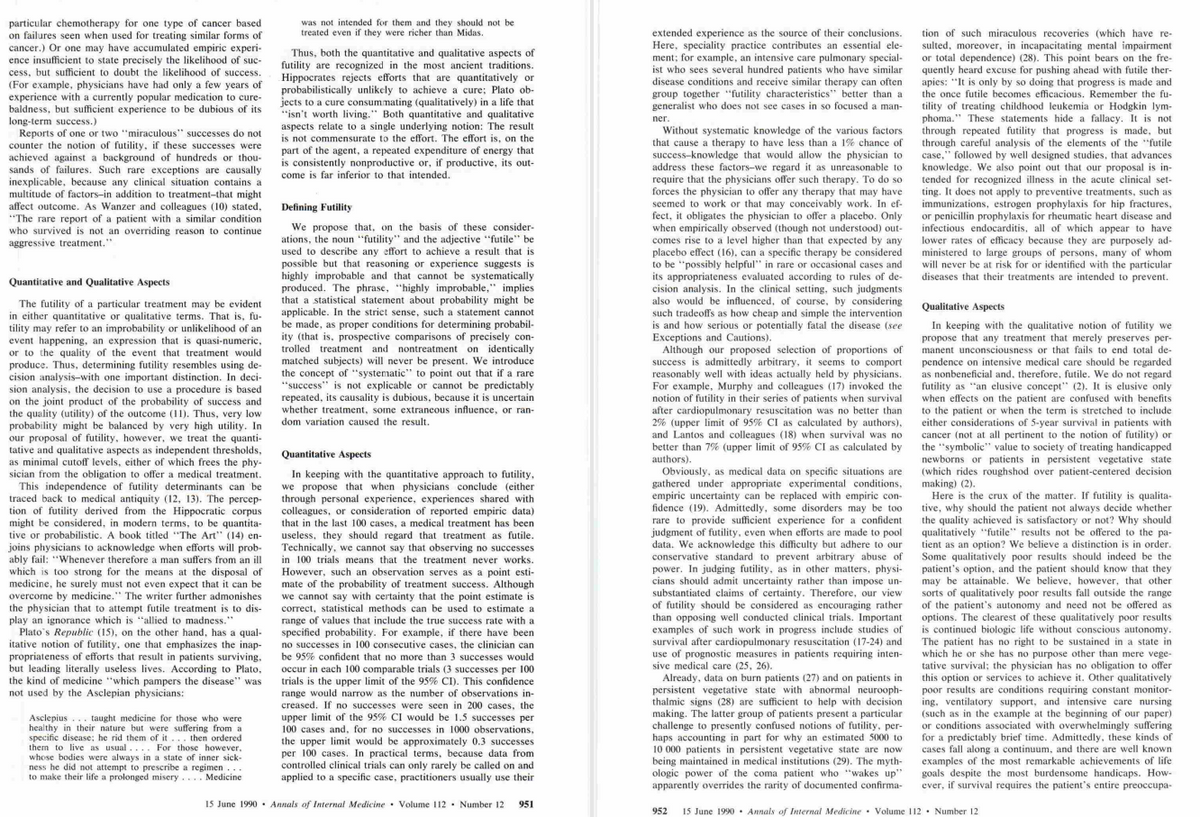
particular chemotherapy for one type of cancer based
on failures seen when used for treating similar forms of
cancer.) Or one may have accumulated empiric experi-
ence insufficient to state precisely the likelihood of suc-
cess, but sufficient to doubt the likelihood of success.
(For example, physicians have had only a few years of
experience with a currently popular medication to cure-
baldness, but sufficient experience to be dubious of its
long-term success.)
Thus, both the quantitative and qualitative aspects of
futility are recognized in the most ancient traditions.
Hippocrates rejects efforts that are quantitatively or
probabilistically unlikely to achieve a cure; Plato ob-
jects to a cure consummating (qualitatively) in a life that
"isn't worth living." Both quantitative and qualitative
aspects relate to a single underlying notion: The result
is not commensurate to the effort. The effort is, on the
part of the agent, a repeated expenditure of energy that
is consistently nonproductive or, if productive, its out-
come is far inferior to that intended.
Reports of one or two "miraculous" successes do not
counter the notion of futility, if these successes were
achieved against a background of hundreds or thou-
sands of failures. Such rare exceptions are causally
inexplicable, because any clinical situation contains a
multitude of factors-in addition to treatment-that might
affect outcome. As Wanzer and colleagues (10) stated,
"The rare report of a patient with a similar condition
who survived is not an overriding reason to continue
aggressive treatment."
Defining Futility
Quantitative and Qualitative Aspects
The futility of a particular treatment may be evident
in either quantitative or qualitative terms. That is, fu-
tility may refer to an improbability or unlikelihood of an
event happening, an expression that is quasi-numeric,
or to the quality of the event that treatment would
produce. Thus, determining futility resembles using de-
cision analysis-with one important distinction. In deci-
sion analysis, the decision to use a procedure is based
on the joint product of the probability of success and
the quality (utility) of the outcome (11). Thus, very low
probability might be balanced by very high utility. In
our proposal of futility, however, we treat the quanti-
tative and qualitative aspects as independent thresholds,
as minimal cutoff levels, either of which frees the phy-
sician from the obligation to offer a medical treatment.
We propose that, on the basis of these consider-
ations, the noun "futility" and the adjective "futile" be
used to describe any effort to achieve a result that is
possible but that reasoning or experience suggests is
highly improbable and that cannot be systematically
produced. The phrase, "highly improbable," implies
that a statistical statement about probability might be
applicable. In the strict sense, such a statement cannot
be made, as proper conditions for determining probabil-
ity (that is, prospective comparisons of precisely con-
trolled treatment and nontreatment on identically
matched subjects) will never be present. We introduce
the concept of "systematic" to point out that if a rare
"success" is not explicable or cannot be predictably
repeated, its causality is dubious, because it is uncertain
whether treatment, some extraneous influence, or ran-
dom variation caused the result.
Quantitative Aspects
This independence of futility determinants can be
traced back to medical antiquity (12, 13). The percep-
tion of futility derived from the Hippocratic corpus.
might be considered, in modern terms, to be quantita-
tive or probabilistic. A book titled "The Art" (14) en-
joins physicians to acknowledge when efforts will prob-
ably fail: "Whenever therefore a man suffers from an ill
which is too strong for the means at the disposal of
medicine, he surely must not even expect that it can be
overcome by medicine." The writer further admonishes
the physician that to attempt futile treatment is to dis-
play an ignorance which is "allied to madness."
In keeping with the quantitative approach to futility,
we propose that when physicians conclude (either
through personal experience, experiences shared with
colleagues, or consideration of reported empiric data)
that in the last 100 cases, a medical treatment has been
useless, they should regard that treatment as futile.
Technically, we cannot say that observing no successes
in 100 trials means that the treatment never works.
However, such an observation serves as a point esti-
mate of the probability of treatment success. Although
we cannot say with certainty that the point estimate is
correct, statistical methods can be used to estimate a
range of values that include the true success rate with a
specified probability. For example, if there have been
no successes in 100 consecutive cases, the clinician can
be 95% confident that no more than 3 successes would
occur in each 100 comparable trials (3 successes per 100
trials is the upper limit of the 95% CI). This confidence
range would narrow as the number of observations in-
creased. If no successes were seen in 200 cases, the
upper limit of the 95% CI would be 1.5 successes per
100 cases and, for no successes in 1000 observations,
the upper limit would be approximately 0.3 successes
per 100 cases. In practical terms, because data from
controlled clinical trials can only rarely be called on and
applied to a specific case, practitioners usually use their
Plato's Republic (15), on the other hand, has a qual-
itative notion of futility, one that emphasizes the inap-
propriateness of efforts that result in patients surviving,
but leading literally useless lives. According to Plato,
the kind of medicine "which pampers the disease" was
not used by the Asclepian physicians:
Asclepius taught medicine for those who were
healthy in their nature but were suffering from a
specific disease; he rid them of it... then ordered
them to live as usual.... For those however,
whose bodies were always in a state of inner sick-
ness he did not attempt to prescribe a regimen ...
to make their life a prolonged misery
Medicine
15 June 1990. Annals of Internal Medicine Volume 112. Number 12 951
tion of such miraculous recoveries (which have re-
sulted, moreover, in incapacitating mental impairment
or total dependence) (28). This point bears on the fre-
quently heard excuse for pushing ahead with futile ther-
apies: "It is only by so doing that progress is made and
the once futile becomes efficacious. Remember the fu-
tility of treating childhood leukemia or Hodgkin lym-
phoma." These statements hide a fallacy. It is not.
through repeated futility that progress is made, but
through careful analysis of the elements of the "futile
case," followed by well designed studies, that advances.
knowledge. We also point out that our proposal is in-
tended for recognized illness in the acute clinical set-
ting. It does not apply to preventive treatments, such as
immunizations, estrogen prophylaxis for hip fractures,
or penicillin prophylaxis for rheumatic heart disease and
infectious endocarditis, all of which appear to have
lower rates of efficacy because they are purposely ad-
ministered to large groups of persons, many of whom
will never be at risk for or identified with the particular
diseases that their treatments are intended to prevent.
Qualitative Aspects
In keeping with the qualitative notion of futility we
propose that any treatment that merely preserves per-
manent unconsciousness or that fails to end total de-
pendence on intensive medical care should be regarded
as nonbeneficial and, therefore, futile. We do not regard
futility as "an elusive concept" (2). It is elusive only
when effects on the patient are confused with benefits.
to the patient or when the term is stretched to include
either considerations of 5-year survival in patients with
cancer (not at all pertinent to the notion of futility) or
the "symbolic" value to society of treating handicapped
newborns or patients in persistent vegetative state
(which rides roughshod over patient-centered decision
making) (2).
Here is the crux of the matter. If futility is qualita-
tive, why should the patient not always decide whether
the quality achieved is satisfactory or not? Why should
qualitatively "futile" results not be offered to the pa-
tient as an option? We believe a distinction is in order.
Some qualitatively poor results should indeed be the
patient's option, and the patient should know that they
may be attainable. We believe, however, that other.
sorts of qualitatively poor results fall outside the range
of the patient's autonomy and need not be offered as
options. The clearest of these qualitatively poor results
is continued biologic life without conscious autonomy.
The patient has no right to be sustained in a state in
which he or she has no purpose other than mere vege-
tative survival; the physician has no obligation to offer
this option or services to achieve it. Other qualitatively
poor results are conditions requiring constant monitor-
ing, ventilatory support, and intensive care nursing
(such as in the example at the beginning of our paper).
or conditions associated with overwhelmingly suffering
for a predictably brief time. Admittedly, these kinds of
cases fall along a continuum, and there are well known
examples of the most remarkable achievements of life
goals despite the most burdensome handicaps. How-
ever, if survival requires the patient's entire preoccupa-
extended experience as the source of their conclusions.
Here, speciality practice contributes an essential ele-
ment; for example, an intensive care pulmonary special-
ist who sees several hundred patients who have similar
disease conditions and receive similar therapy can often
group together "futility characteristics" better than at
generalist who does not see cases in so focused a man-
ner.
Without systematic knowledge of the various factors
that cause a therapy to have less than a 1% chance of
success-knowledge that would allow the physician to
address these factors-we regard it as unreasonable to
require that the physicians offer such therapy. To do so
forces the physician to offer any therapy that may have
seemed to work or that may conceivably work. In ef-
fect, it obligates the physician to offer a placebo. Only
when empirically observed (though not understood) out-
comes rise to a level higher than that expected by any
placebo effect (16), can a specific therapy be considered
to be "possibly helpful" in rare or occasional cases and
its appropriateness evaluated according to rules of de-
cision analysis. In the clinical setting, such judgments
also would be influenced, of course, by considering
such tradeoffs as how cheap and simple the intervention
is and how serious or potentially fatal the disease (see
Exceptions and Cautions).
Although our proposed selection of proportions of
success is admittedly arbitrary, it seems to comport
reasonably well with ideas actually held by physicians.
For example, Murphy and colleagues (17) invoked the
notion of futility in their series of patients when survival
after cardiopulmonary resuscitation was no better than
2% (upper limit of 95% CI as calculated by authors),
and Lantos and colleagues (18) when survival was no
better than 7% (upper limit of 95% CI as calculated by
authors).
Obviously, as medical data on specific situations are
gathered under appropriate experimental conditions,
empiric uncertainty can be replaced with empiric con-
fidence (19). Admittedly, some disorders may be too.
rare to provide sufficient experience for a confident
judgment of futility, even when efforts are made to pool
data. We acknowledge this difficulty but adhere to our
conservative standard to prevent arbitrary abuse of
power. In judging futility, as in other matters, physi-
cians should admit uncertainty rather than impose un-
substantiated claims of certainty. Therefore, our view
of futility should be considered as encouraging rather
than opposing well conducted clinical trials. Important
examples of such work in progress include studies of
survival after cardiopulmonary resuscitation (17-24) and
use of prognostic measures in patients requiring inten-
sive medical care (25, 26).
Already, data on burn patients (27) and on patients in
persistent vegetative state with abnormal neurooph-
thalmic signs (28) are sufficient to help with decision
making. The latter group of patients present a particular
challenge to presently confused notions of futility, per-
haps accounting in part for why an estimated 5000 to
10 000 patients in persistent vegetative state are now
being maintained in medical institutions (29). The myth-
ologic power of the coma patient who "wakes up".
apparently overrides the rarity of documented confirma-
952 15 June 1990 Annals of Internal Medicine Volume 112 Number 12

Transcribed Image Text:tion with intensive medical treatment, to the extent that
he or she cannot achieve any other life goals (thus
obviating the goal of medical care), the treatment is
effective but not beneficial; it need not be offered to the
patient, and the patient's family has no right to demand
it.
Specifically excluded from our concept of futility is
medical care for patients for whom such care offers the
opportunity to achieve life goals, however limited.
Thus, patients whose illnesses are severe enough to
require frequent hospitalization, patients confined to
nursing homes, or patients with severe physical or men-
tal handicaps are not, in themselves, objects of futile
treatments. Such patients (or their surrogates) have the
right to receive or reject any medical treatment accord-
ing to their own perceptions of benefits compared with
burdens.
Some observers might object, as a matter of princi-
ple, to excluding patient input from assessments of
qualitative futility. Others might be concerned that such
exclusion invites abuse, neglect, and a retreat to the
paternalistic "silent world" of the past in which doctors
avoided communication with their patients (30). In re-
sponse to the latter objection, we acknowledge that
potential for abuse is present and share this concern.
We would deplore the use of our proposal to excuse
physicians from engaging patients in ongoing informed
dialogue. Nonetheless, the alternative is also subject to
abuse (for example, when legal threats made by patients
and surrogates cow hospitals into providing excessive
care). We reiterate that the distinction between medical
benefit and effect justifies excluding patients from de-
termination of qualitative futility. Physicians are re-
quired only to provide medical benefits to patients. Phy-
sicians are permitted, but not obligated, to offer other.
non-medical benefits. For example, a physician is not
obligated to keep a patient alive in an irreversible veg-
etative state, because doing so does not medically ben-
efit the patient. However, as noted below, a physician
may do so on compassionate grounds, when temporary
continuance of biologic life achieves goals of the patient
or family.
Exceptions and Cautions
We have attempted to provide a working definition of
futility. We also have drawn attention to the ethical
notion that futility is a professional judgment that takes
precedence over patient autonomy and permits physi-
cians to withhold or withdraw care deemed to be inap-
propriate without subjecting such a decision to patient
approval. Thus, we regard our proposal as representing
the ordinary duties of physicians, duties that are appli-
cable where there is medical agreement that the de-
scribed standards of futility are met. We recognize,
however, that the physician's duty to serve the best
interests of the patient may require that exceptions to
our approaches be made under special circumstances.
An exception could well be made out of compassion
for the patient with terminal metastatic cancer who re-
quests resuscitation in the event of cardiac arrest to
survive long enough to see a son or daughter who has
not yet arrived from afar to pay last respects. Such an
exception could also be justified to facilitate coping and
grieving by family members, a goal the patient might
support (32-36). Although resuscitation may be clearly
futile (that is, would keep the patient alive in the inten-
sive care unit for only 1 or 2 more days), complying
with the patient's wishes would be appropriate, pro-
vided such exceptions do not impose undue burdens on
other patients, health care providers, and the institu-
tion, by directly threatening the health care of others.
We hasten to add, however, that our notion of futility
does not arise from considerations of scarce resources.
Arguments for limiting treatments on grounds of re-
source allocation should proceed by an entirely different
route and with great caution in our present open system
of medical care, as there is no universally accepted
value system for allocation (31) and no guarantee that
any limits a physician imposes on his or her patients
will be equitably shared by other physicians and pa-
tients in the same circumstances (37, 38).
Admittedly, in cases in which treatment has begun
already, there may be an emotional bias to continue,
rather than withdraw, futile measures (10). If greater
attention is paid at the outset to indicating futile treat-
ments, these situations would occur less frequently;
however, the futility of a given treatment may not be-
come clear until it has been implemented. We submit
that physicians are entitled to cease futile measures in
such cases, but should do so in a manner sensitive to
the emotional investments and concerns of caretakers.
What if a hospitalized patient with advanced cancer
demands a certain medication (for example, a particular
vitamin), a treatment that the physician believes to be
futile? Several aspects of this demand support its over-
riding the physician's invocation of futility. Certain
death is expected and, although an objective goal such
as saving the patient's life or even releasing the patient
from the hospital might be unachievable, the subjective
goal of patient well-being might be enhanced (a placebo-
induced benefit). In this particular situation, the effort
and resources invested to achieve this goal impose a
negligible burden on the health care system and do not
threaten the health care of others. Thus, although phy-
sicians are not obligated to offer a placebo, they occa-
sionally do. For example, Imbus and Zawacki (27) al-
lowed burn patients to opt for treatment even when
survival was unprecedented. In this clinical situation,
compassionate yielding imposes no undue burden, be-
cause survival with or without treatment is measured in
days. In contrast, yielding to a surrogate's demand for
unlimited life-support for a patient in persistent vegeta-
tive state may lead to decades of institutional care.
Acknowledgments: The authors thank two anonymous reviewers and
Robert M. Kaplan, PhD, for their helpful comments.
Requests for Reprints: Lawrence J. Schneiderman, MD, University of
California, San Diego. School of Medicine, Department of Community
and Family Medicine, M-022, La Jolla, CA 92093.
Current Author Addresses: Dr. Schneiderman: University of California.
San Diego, School of Medicine. Department of Community and Family
Medicine. M-022. La Jolla. CA 92093.
Drs. Jecker and Jonsen: School of Medicine, SB-20, University of
Washington, Seattle, WA 98195.
Expert Solution
This question has been solved!
Explore an expertly crafted, step-by-step solution for a thorough understanding of key concepts.
This is a popular solution!
Trending now
This is a popular solution!
Step by step
Solved in 3 steps
Recommended textbooks for you

Biology: The Unity and Diversity of Life (MindTap…
Biology
ISBN:
9781305073951
Author:
Cecie Starr, Ralph Taggart, Christine Evers, Lisa Starr
Publisher:
Cengage Learning

Human Biology (MindTap Course List)
Biology
ISBN:
9781305112100
Author:
Cecie Starr, Beverly McMillan
Publisher:
Cengage Learning
Biology: The Unity and Diversity of Life (MindTap…
Biology
ISBN:
9781337408332
Author:
Cecie Starr, Ralph Taggart, Christine Evers, Lisa Starr
Publisher:
Cengage Learning

Biology: The Unity and Diversity of Life (MindTap…
Biology
ISBN:
9781305073951
Author:
Cecie Starr, Ralph Taggart, Christine Evers, Lisa Starr
Publisher:
Cengage Learning

Human Biology (MindTap Course List)
Biology
ISBN:
9781305112100
Author:
Cecie Starr, Beverly McMillan
Publisher:
Cengage Learning
Biology: The Unity and Diversity of Life (MindTap…
Biology
ISBN:
9781337408332
Author:
Cecie Starr, Ralph Taggart, Christine Evers, Lisa Starr
Publisher:
Cengage Learning