Surgical Tech For Surgical Tech Pos Care
5th Edition
ISBN:9781337648868
Author:Association
Publisher:Association
Chapter9: Surgical Pharmacology And Anesthesia
Section: Chapter Questions
Problem 2CS
Related questions
Question
1. Create a Client Centered Pathophysiology.
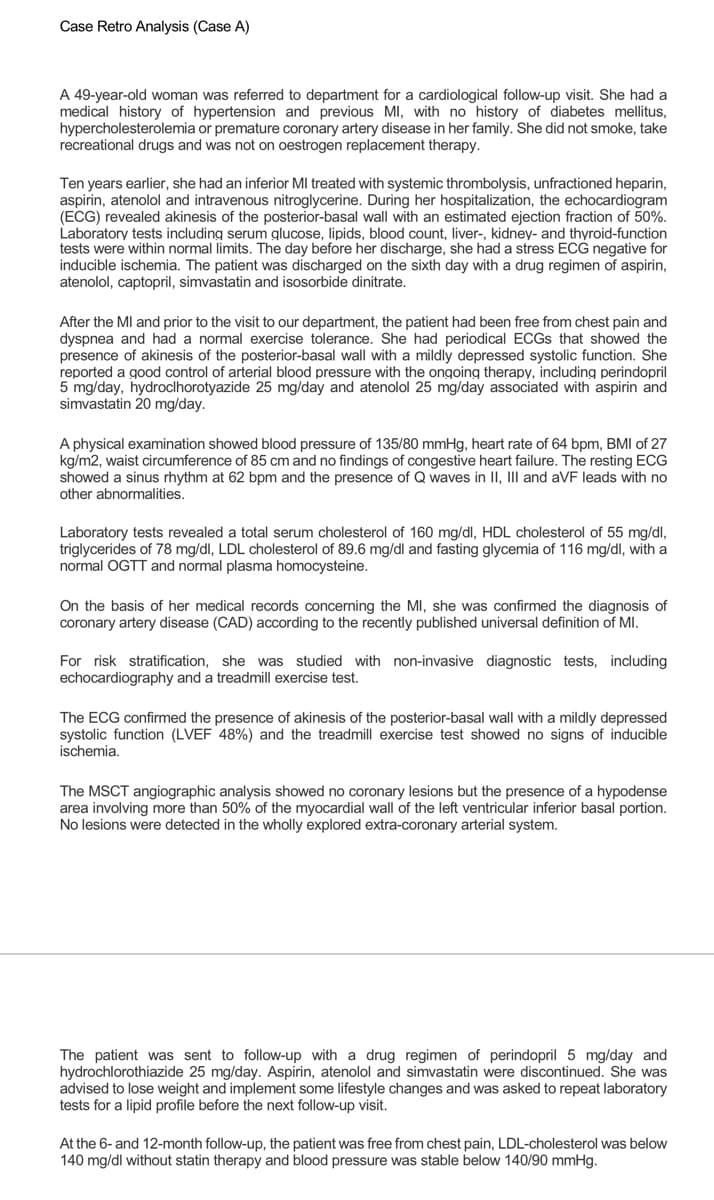
Transcribed Image Text:Case Retro Analysis (Case A)
A 49-year-old woman was referred to department for a cardiological follow-up visit. She had a
medical history of hypertension and previous MI, with no history of diabetes mellitus,
hypercholesterolemia or premature coronary artery disease in her family. She did not smoke, take
recreational drugs and was not on oestrogen replacement therapy.
Ten years earlier, she had an inferior MI treated with systemic thrombolysis, unfractioned heparin,
aspirin, atenolol and intravenous nitroglycerine. During her hospitalization, the echocardiogram
(ECG) revealed akinesis of the posterior-basal wall with an estimated ejection fraction of 50%.
Laboratory tests including serum glucose, lipids, blood count, liver-, kidney- and thyroid-function
tests were within normal limits. The day before her discharge, she had a stress ECG negative for
inducible ischemia. The patient was discharged on the sixth day with a drug regimen of aspirin,
atenolol, captopril, simvastatin and isosorbide dinitrate.
After the MI and prior to the visit to our department, the patient had been free from chest pain and
dyspnea and had a normal exercise tolerance. She had periodical ECGS that showed the
presence of akinesis of the posterior-basal wall with a mildly depressed systolic function. She
reported a good control of arterial blood pressure with the ongoing therapy, including perindopril
5 mg/day, hydroclhorotyazide 25 mg/day and atenolol 25 mg/day associated with aspirin and
simvastatin 20 mg/day.
A physical examination showed blood pressure of 135/80 mmHg, heart rate of 64 bpm, BMI of 27
kg/m2, waist circumference of 85 cm and no findings of congestive heart failure. The resting ECG
showed a sinus rhythm at 62 bpm and the presence of Q waves in II, III and aVF leads with no
other abnormalities.
Laboratory tests revealed a total serum cholesterol of 160 mg/dl, HDL cholesterol of 55 mg/dl,
triglycerides of 78 mg/dl, LDL cholesterol of 89.6 mg/dl and fasting glycemia of 116 mg/dl, with a
normal OGTT and normal plasma homocysteine.
On the basis of her medical records concerning the MI, she was confirmed the diagnosis of
coronary artery disease (CAD) according to the recently published universal definition of MI.
For risk stratification, she was studied with non-invasive diagnostic tests, including
echocardiography and a treadmill exercise test.
The ECG confirmed the presence of akinesis of the posterior-basal wall with a mildly depressed
systolic function (LVEF 48%) and the treadmill exercise test showed no signs of inducible
ischemia.
The MSCT angiographic analysis showed no coronary lesions but the presence of a hypodense
area involving more than 50% of the myocardial wall of the left ventricular inferior basal portion.
No lesions were detected in the wholly explored extra-coronary arterial system.
The patient was sent to follow-up with a drug regimen of perindopril 5 mg/day and
hydrochlorothiazide 25 mg/day. Aspirin, atenolol and simvastatin were discontinued. She was
advised to lose weight and implement some lifestyle changes and was asked to repeat laboratory
tests for a lipid profile before the next follow-up visit.
At the 6- and 12-month follow-up, the patient was free from chest pain, LDL-cholesterol was below
140 mg/dl without statin therapy and blood pressure was stable below 140/90 mmHg.
Expert Solution
This question has been solved!
Explore an expertly crafted, step-by-step solution for a thorough understanding of key concepts.
Step by step
Solved in 3 steps
Recommended textbooks for you

Surgical Tech For Surgical Tech Pos Care
Health & Nutrition
ISBN:
9781337648868
Author:
Association
Publisher:
Cengage

Essentials of Pharmacology for Health Professions
Nursing
ISBN:
9781305441620
Author:
WOODROW
Publisher:
Cengage


Surgical Tech For Surgical Tech Pos Care
Health & Nutrition
ISBN:
9781337648868
Author:
Association
Publisher:
Cengage

Essentials of Pharmacology for Health Professions
Nursing
ISBN:
9781305441620
Author:
WOODROW
Publisher:
Cengage

