Can S-layer proteins be detected by immunolabelling when a capsule is present? How do you know? I need help finding the answer in the article and explain in short answer
Can S-layer proteins be detected by immunolabelling when a capsule is present? How do you know? I need help finding the answer in the article and explain in short answer
Basic Clinical Laboratory Techniques 6E
6th Edition
ISBN:9781133893943
Author:ESTRIDGE
Publisher:ESTRIDGE
Chapter4: Basic Immunology And Immunohematology
Section4.6: Abo Grouping
Problem 7RQ
Related questions
Question
Can S-layer proteins be detected by immunolabelling when a capsule is present? How do you know?
I need help finding the answer in the article and explain in short answer
link to article: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC106848/
Transcribed Image Text:Capsule observation. The aspect and homogeneity of capsulation were
checked by India ink exclusion (4).
Electron microscopy. (i) Thin sections. Cells were fixed with 2% formaldehyde
(made freshly from paraformaldehyde) and 2.5% glutaraldehyde in 0.1 M caco-
dylate buffer (pH 7.2) containing 5 mM CaCl₂ (14, 17). After being washed, the
cells were postfixed for 2 h with 2% OsO4 in the same buffer. The pelleted
bacteria were embedded in 2% low-melting-point agar (type IX; Sigma) (36).
The samples were then treated for 16 h with 0.5% uranyl acetate in water. After
extensive washing, small blocks were dehydrated with alcohol and embedded in
Spurr's medium (Ladd Inc.) (32). Thin sections were stained conventionally and
observed with a Philips CM12 electron microscope.
(ii) Immunocytochemistry with thin sections. B. anthracis cells were fixed with
2% formaldehyde and 0.2% glutaraldehyde in 0.1 M phosphate-buffered saline
(14 mM Na₂HPO4, 7 mM NaH₂PO4, 150 mM NaCl) (PBS) (pH 7.4) for 1 h,
rinsed in the same buffer, and embedded in 2% low-melting-point agar (36).
Small blocks containing bacteria were embedded in Lowicryl HM20 (Poly-
sciences Ltd.) at -50°C following the progressively lower temperatures protocol
of Carlemalm et al. (3) as described by Newman and Hobot (25). Thin sections
were collected onto Formvar-carbon-coated nickel grids and incubated succes-
sively at room temperature with the following solutions: PBS-50 mM NH4Cl for
10 min; PBS-1% bovine serum albumin (BSA)-1% normal goat serum-0.1%
Tween 20 for 10 min; specific anti-EA1 or anti-Sap antibodies diluted 1/50 in
PBS-1% BSA-1% normal goat serum-0.1% Tween 20 for 1 h; PBS-0.1% BSA
three times for 5 min each time; goat immunoglobulin G (heavy and light chains)
anti-rabbit immunoglobulin-gold conjugate diluted 1/20 in PBS-0.01% gelatin
for 1 h; PBS three times for 5 min each time; PBS-1% glutaraldehyde for 5 min;
and five times with water. The thin sections were then stained by incubation with
2% uranyl acetate in water for 35 min and then in lead tartrate for 2 min (23).
(iii) Immunocytochemistry with whole-mount cells. Immunocytochemistry
with whole-mount cells was carried out as previously described (20).
(iv) Negative staining experiments. B. anthracis cells were resuspended in a
1/10 volume of 25 mM Tris-HCl (pH 8.0)–10 mM MgCl₂ with 0.25 or 0.5%
glutaraldehyde for EA1 or Sap, respectively, in the presence of approximately 30
μl of 425- to 600-µm glass beads (Sigma) and disrupted by vortexing for 30 s. This
treatment disintegrated the capsule. Negative staining was performed as previ-
ously described (20). Micrographs were recorded with a Philips CM12 electron
microscope under low-dose (17 electrons/Å/s) transmission electron microscopy
conditions.
RESULTS
Cosynthesis and respective localization of the capsule and
the S-layer components. All reported data on the B. anthracis
S-layer is from noncapsulated strains (6, 7, 10, 16, 20). We
therefore investigated whether the capsule and the S-layer
components, EA1 and Sap, could all be simultaneously
present. The genes for EA1 and Sap are chromosomal and
have been well characterized for the plasmid-free strain 9131
S
0
A
B
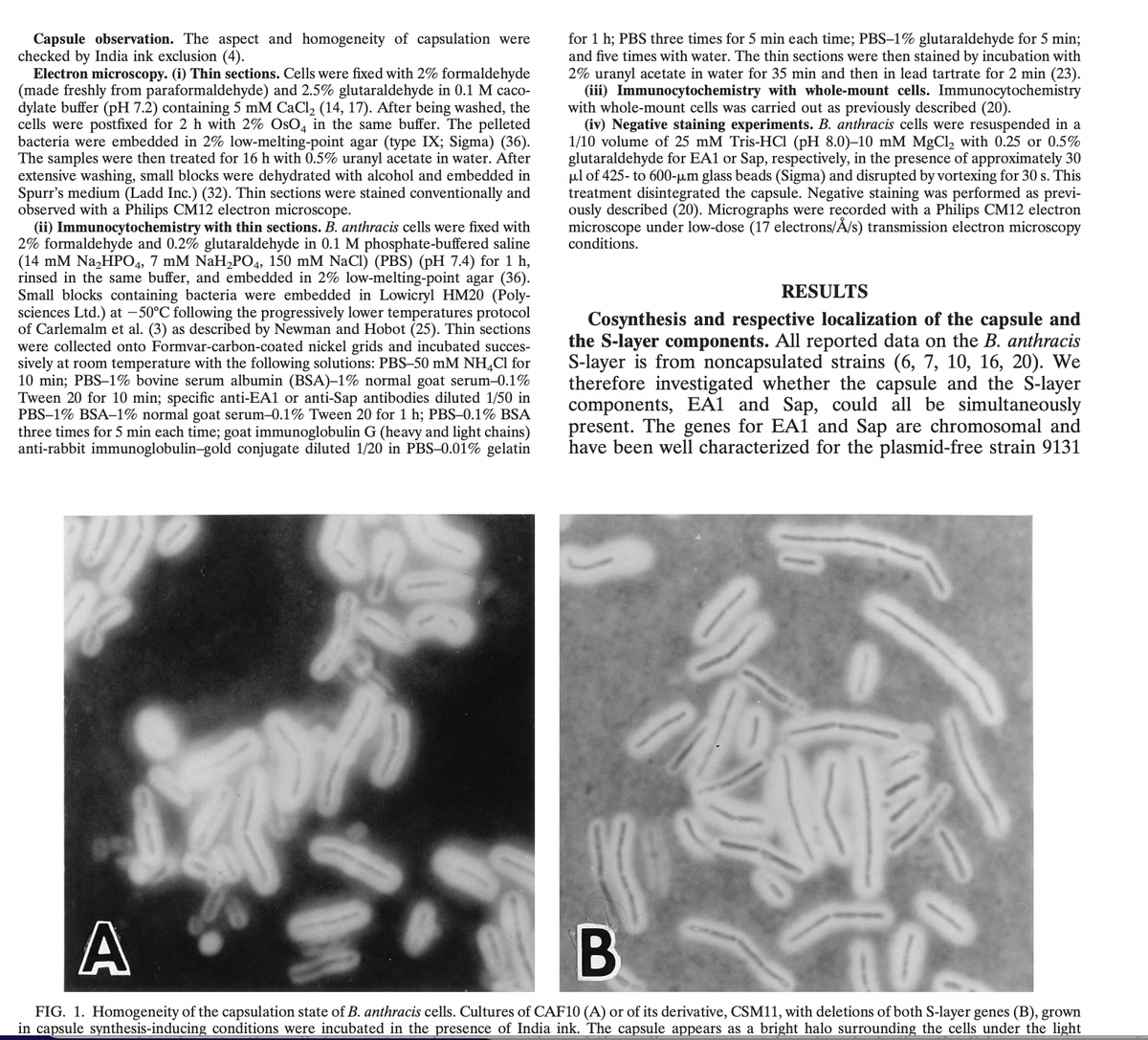
FIG. 1. Homogeneity of the capsulation state of B. anthracis cells. Cultures of CAF10 (A) or of its derivative, CSM11, with deletions of both S-layer genes (B), grown
in capsule synthesis-inducing conditions were incubated in the presence of India ink. The capsule appears as a bright halo surrounding the cells under the light
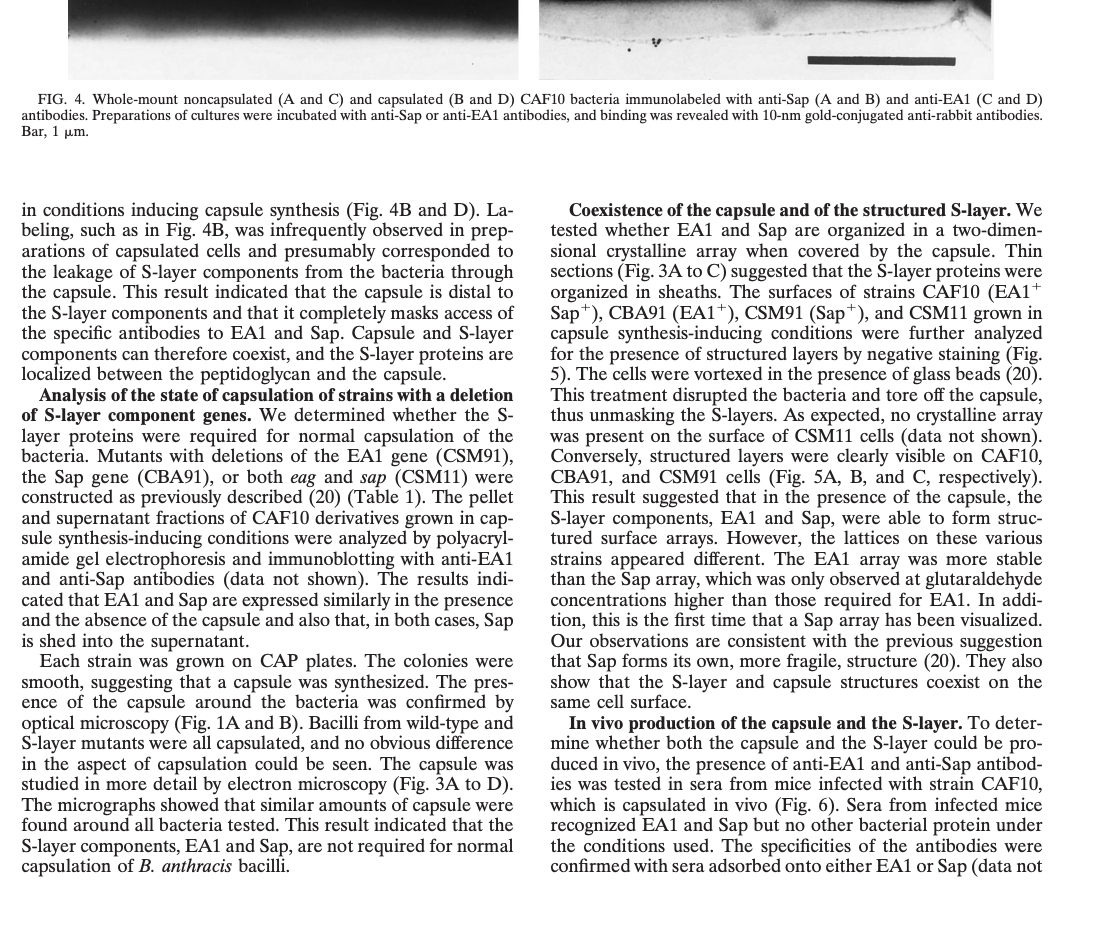
Transcribed Image Text:FIG. 4. Whole-mount noncapsulated (A and C) and capsulated (B and D) CAF10 bacteria immunolabeled with anti-Sap (A and B) and anti-EA1 (C and D)
antibodies. Preparations of cultures were incubated with anti-Sap or anti-EA1 antibodies, and binding was revealed with 10-nm gold-conjugated anti-rabbit antibodies.
Bar, 1 µm.
in conditions inducing capsule synthesis (Fig. 4B and D). La-
beling, such as in Fig. 4B, was infrequently observed in prep-
arations of capsulated cells and presumably corresponded to
the leakage of S-layer components from the bacteria through
the capsule. This result indicated that the capsule is distal to
the S-layer components and that it completely masks access of
the specific antibodies to EA1 and Sap. Capsule and S-layer
components can therefore coexist, and the S-layer proteins are
localized between the peptidoglycan and the capsule.
Analysis of the state of capsulation of strains with a deletion
of S-layer component genes. We determined whether the S-
layer proteins were required for normal capsulation of the
bacteria. Mutants with deletions of the EA1 gene (CSM91),
the Sap gene (CBA91), or both eag and sap (CSM11) were
constructed as previously described (20) (Table 1). The pellet
and supernatant fractions of CAF10 derivatives grown in cap-
sule synthesis-inducing conditions were analyzed by polyacryl-
amide gel electrophoresis and immunoblotting with anti-EA1
and anti-Sap antibodies (data not shown). The results indi-
cated that EA1 and Sap are expressed similarly in the presence
and the absence of the capsule and also that, in both cases, Sap
is shed into the supernatant.
Each strain was grown on CAP plates. The colonies were
smooth, suggesting that a capsule was synthesized. The pres-
ence of the capsule around the bacteria was confirmed by
optical microscopy (Fig. 1A and B). Bacilli from wild-type and
S-layer mutants were all capsulated, and no obvious difference
in the aspect of capsulation could be seen. The capsule was
studied in more detail by electron microscopy (Fig. 3A to D).
The micrographs showed that similar amounts of capsule were
found around all bacteria tested. This result indicated that the
S-layer components, EA1 and Sap, are not required for normal
capsulation of B. anthracis bacilli.
Coexistence of the capsule and of the structured S-layer. We
tested whether EA1 and Sap are organized in a two-dimen-
sional crystalline array when covered by the capsule. Thin
sections (Fig. 3A to C) suggested that the S-layer proteins were
organized in sheaths. The surfaces of strains CAF10 (EA1+
Sap), CBA91 (EA1+), CSM91 (Sap), and CSM11 grown in
capsule synthesis-inducing conditions were further analyzed
for the presence of structured layers by negative staining (Fig.
5). The cells were vortexed in the presence of glass beads (20).
This treatment disrupted the bacteria and tore off the capsule,
thus unmasking the S-layers. As expected, no crystalline array
was present on the surface of CSM11 cells (data not shown).
Conversely, structured layers were clearly visible on CAF10,
CBA91, and CSM91 cells (Fig. 5A, B, and C, respectively).
This result suggested that in the presence of the capsule, the
S-layer components, EA1 and Sap, were able to form struc-
tured surface arrays. However, the lattices on these various
strains appeared different. The EA1 array was more stable
than the Sap array, which was only observed at glutaraldehyde
concentrations higher than those required for EA1. In addi-
tion, this is the first time that a Sap array has been visualized.
Our observations are consistent with the previous suggestion
that Sap forms its own, more fragile, structure (20). They also
show that the S-layer and capsule structures coexist on the
same cell surface.
In vivo production of the capsule and the S-layer. To deter-
mine whether both the capsule and the S-layer could be pro-
duced in vivo, the presence of anti-EA1 and anti-Sap antibod-
ies was tested in sera from mice infected with strain CAF10,
which is capsulated in vivo (Fig. 6). Sera from infected mice
recognized EA1 and Sap but no other bacterial protein under
the conditions used. The specificities of the antibodies were
confirmed with sera adsorbed onto either EA1 or Sap (data not
Expert Solution
This question has been solved!
Explore an expertly crafted, step-by-step solution for a thorough understanding of key concepts.
Step by step
Solved in 2 steps
Knowledge Booster
Learn more about
Need a deep-dive on the concept behind this application? Look no further. Learn more about this topic, biology and related others by exploring similar questions and additional content below.Recommended textbooks for you

