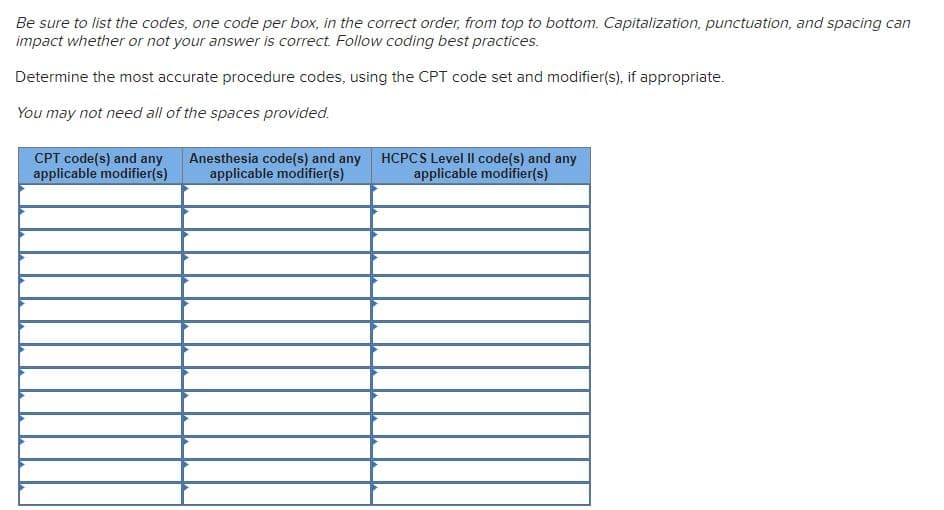
Using the coding techniques described in this chapter, carefully read through the case study and determine the most accurate CPT code(s) and HCPCS code(s) and modifier(s), if appropriate. EMERGENCY DEPARTMENT HISTORY OF PRESENT ILLNESS: The patient came in today for possible reaction to immunotherapy. She has been seeing Dr. Oligby for allergic rhinitis and asthma. She states that she is currently building on immunotherapy and yesterday received injections with oak/birch/maple 100 PNU 0.3 mL, grass and ragweed 100 BAU 0.3 mL, cat/dog 50 BAU 0.3 mL, and mite and mold mix 100 units 0.3 mL. The patient tells me after the immunotherapy, she went home and within hours felt some chest tightness. The patient used her albuterol inhaler, but the chest tightness got worse and she ended up taking her Symbicort 160/4.5 two puffs as well as some Claritin. She continued to feel lethargic and out of breath. She also had an itchy area on her left arm where she received the cat/dog injection. She was able to go to sleep that night but woke twice due to wheezing and used her albuterol inhaler and went back to sleep. When she woke up this morning, she was very tired and dizzy and could not catch her breath. She used her albuterol inhaler once or twice this morning as well as the Symbicort and took a tablet of Zyrtec. Then, around 9 or 9:30, when she was at work, she felt her tongue swelling. During this time, she felt she couldn’t breathe normally. The albuterol inhaler did not have any benefit; neither did the other medications she tried. She tells me she had no rash, hives, or vomiting and is not coughing. She tells me she has not been sick this week. No fever. She has been off of her Symbicort since November because she felt her asthma is fine. She has had no recent trouble with asthma. No recent exposure to animals, dust, or other allergens. She is on no new medications. She has no pets at home and continues to avoid turkey and chicken and has no new foods during this time. She has a history of anxiety and panic attacks and does feel she is having one now. MEDICATIONS: Topamax for migraine headaches, Lexapro ALLERGIES: NKDA PHYSICAL EXAMINATION: GENERAL: The patient is a healthy-appearing, well-nourished, well-developed 45-year-old female in no acute distress but does appear to be breathing heavy and very shaky and panicky. VITAL SIGNS: Height is 63 inches. Weight is 132 pounds. Blood pressure is 106/70. HEENT: Tympanic membranes are normal. Throat is clear. I did not appreciate any swelling of the tongue or angioedema. NECK: Supple without adenopathy LUNGS: Completely clear HEART: Regular rate and rhythm without murmur STUDIES: I administered spirometry when she was a little bit more relaxed and achieved an FEV1 of 3.1 liters or 88% of predicted, FEF25–75 is 118% of predicted. Graphic record was placed in patient’s chart. IMPRESSION: 1. The patient appears to be having some anxiety and panic now. It is hard to say whether this started with some mild asthma symptoms as a result of her immunotherapy or if this is purely an anxiety issue. 2. Allergic asthma 3. Allergic rhinitis RECOMMENDATIONS: 1. We recommend a cutback of the dose of immunotherapy at the next visit to oak/birch/maple 100 PNU at 0.2 mL, grass and ragweed 100 BAU at 0.2 mL, cat/dog 50 BAU at 0.2 mL, and mite and mold mix 100 units at 0.2 mL 2. Restart Symbicort 160/4.5 two puffs twice daily 3. Zyrtec 10 mg daily for the next week and prior to immunotherapy 4. Albuterol two puffs every 4 hours as needed 5. The patient should follow up if symptoms do not clear in the next day or two 6. Report to be sent to Dr. Oligby 7. Patient discharged at 16:55
Using the coding techniques described in this chapter, carefully read through the case study and determine the most accurate CPT code(s) and HCPCS code(s) and modifier(s), if appropriate.
EMERGENCY DEPARTMENT
HISTORY OF PRESENT ILLNESS: The patient came in today for possible reaction to immunotherapy. She has been seeing Dr. Oligby for allergic rhinitis and asthma. She states that she is currently building on immunotherapy and yesterday received injections with oak/birch/maple 100 PNU 0.3 mL, grass and ragweed 100 BAU 0.3 mL, cat/dog 50 BAU 0.3 mL, and mite and mold mix 100 units 0.3 mL. The patient tells me after the immunotherapy, she went home and within hours felt some chest tightness. The patient used her albuterol inhaler, but the chest tightness got worse and she ended up taking her Symbicort 160/4.5 two puffs as well as some Claritin. She continued to feel lethargic and out of breath. She also had an itchy area on her left arm where she received the cat/dog injection. She was able to go to sleep that night but woke twice due to wheezing and used her albuterol inhaler and went back to sleep. When she woke up this morning, she was very tired and dizzy and could not catch her breath. She used her albuterol inhaler once or twice this morning as well as the Symbicort and took a tablet of Zyrtec. Then, around 9 or 9:30, when she was at work, she felt her tongue swelling. During this time, she felt she couldn’t breathe normally. The albuterol inhaler did not have any benefit; neither did the other medications she tried. She tells me she had no rash, hives, or vomiting and is not coughing. She tells me she has not been sick this week. No fever. She has been off of her Symbicort since November because she felt her asthma is fine. She has had no recent trouble with asthma. No recent exposure to animals, dust, or other allergens. She is on no new medications. She has no pets at home and continues to avoid turkey and chicken and has no new foods during this time. She has a history of anxiety and panic attacks and does feel she is having one now.
MEDICATIONS: Topamax for migraine headaches, Lexapro
ALLERGIES: NKDA
PHYSICAL EXAMINATION:
GENERAL: The patient is a healthy-appearing, well-nourished, well-developed 45-year-old female in no acute distress but does appear to be breathing heavy and very shaky and panicky.
VITAL SIGNS: Height is 63 inches. Weight is 132 pounds. Blood pressure is 106/70.
HEENT: Tympanic membranes are normal. Throat is clear. I did not appreciate any swelling of the tongue or angioedema.
NECK: Supple without adenopathy
LUNGS: Completely clear
HEART: Regular rate and rhythm without murmur
STUDIES: I administered spirometry when she was a little bit more relaxed and achieved an FEV1 of 3.1 liters or 88% of predicted, FEF25–75 is 118% of predicted. Graphic record was placed in patient’s chart.
IMPRESSION:
1. The patient appears to be having some anxiety and panic now. It is hard to say whether this started with some mild asthma symptoms as a result of her immunotherapy or if this is purely an anxiety issue.
2. Allergic asthma
3. Allergic rhinitis
RECOMMENDATIONS:
1. We recommend a cutback of the dose of immunotherapy at the next visit to oak/birch/maple 100 PNU at 0.2 mL, grass and ragweed 100 BAU at 0.2 mL, cat/dog 50 BAU at 0.2 mL, and mite and mold mix 100 units at 0.2 mL
2. Restart Symbicort 160/4.5 two puffs twice daily
3. Zyrtec 10 mg daily for the next week and prior to immunotherapy
4. Albuterol two puffs every 4 hours as needed
5. The patient should follow up if symptoms do not clear in the next day or two
6. Report to be sent to Dr. Oligby
7. Patient discharged at 16:55
Trending now
This is a popular solution!
Step by step
Solved in 2 steps