When an RH-negative woman is ABO- compatible with her husband, as Mr. and Mrs Waymarsh are, the risk of Rh alloimmunization is 16 percent. When they are ABO incompatible the risk falls to 7 percent. How do you explain this difference?
When an RH-negative woman is ABO- compatible with her husband, as Mr. and Mrs Waymarsh are, the risk of Rh alloimmunization is 16 percent. When they are ABO incompatible the risk falls to 7 percent. How do you explain this difference?
Anatomy & Physiology
1st Edition
ISBN:9781938168130
Author:Kelly A. Young, James A. Wise, Peter DeSaix, Dean H. Kruse, Brandon Poe, Eddie Johnson, Jody E. Johnson, Oksana Korol, J. Gordon Betts, Mark Womble
Publisher:Kelly A. Young, James A. Wise, Peter DeSaix, Dean H. Kruse, Brandon Poe, Eddie Johnson, Jody E. Johnson, Oksana Korol, J. Gordon Betts, Mark Womble
Chapter18: The Cardiovascular System: Blood
Section: Chapter Questions
Problem 39CTQ: In preparation for a scheduled surgery, a patient visits the hospital lab for a blood draw. The...
Related questions
Question
When an RH-negative woman is ABO- compatible with her husband, as Mr. and Mrs Waymarsh are, the risk of Rh alloimmunization is 16 percent. When they are ABO incompatible the risk falls to 7 percent. How do you explain this difference?
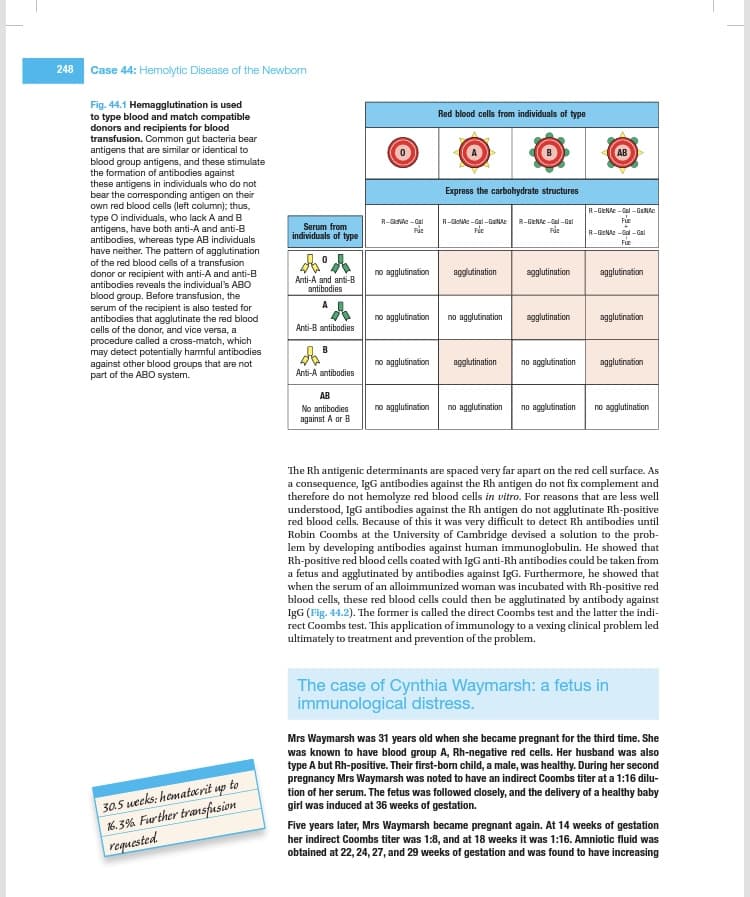
Transcribed Image Text:248
Case 44: Hemolytic Disease of the Newborn
Fig. 44.1 Hemagglutination is used
to type blood and match compatible
donors and recipients for blood
transfusion. Common gut bacteria bear
antigens that are similar or identical to
blood group antigens, and these stimulate
the formation of antibodies against
these antigens in individuals who do not
bear the corresponding antigen on their
own red blood cells (left column); thus,
type O individuals, who lack A and B
antigens, have both anti-A and anti-B
antibodies, whereas type AB individuals
have neither. The pattern of agglutination
of the red blood cells of a transfusion
donor or recipient with anti-A and anti-B
antibodies reveals the individual's ABO
blood group. Before transfusion, the
serum of the recipient is also tested for
antibodies that agglutinate the red blood
cells of the donor, and vice versa, a
procedure called a cross-match, which
may detect potentially harmful antibodies
against other blood groups that are not
part of the ABO system.
30.5 weeks: hematocrit up to
16.3% Further transfusion
requested.
Serum from
individuals of type
Anti-A and anti-B
antibodies
Anti-B antibodies
B
Anti-A antibodies
AB
No antibodies
against A or B
R-GlcNAc-Gal
Fue
no agglutination
no agglutination
no agglutination
no agglutination
Red blood cells from individuals of type
Express the carbohydrate structures
R-GlcNAc-Gal-GalNAc R-GlcNAc-Gal-Gal
Fúc
Ric
agglutination
no agglutination
agglutination
no agglutination
agglutination
agglutination
no agglutination
no agglutination
R-GlcNAc-Gal-GaNAC
3-2.3-2
R-GNA-Gal-Gal
agglutination
agglutination
agglutination
no agglutination
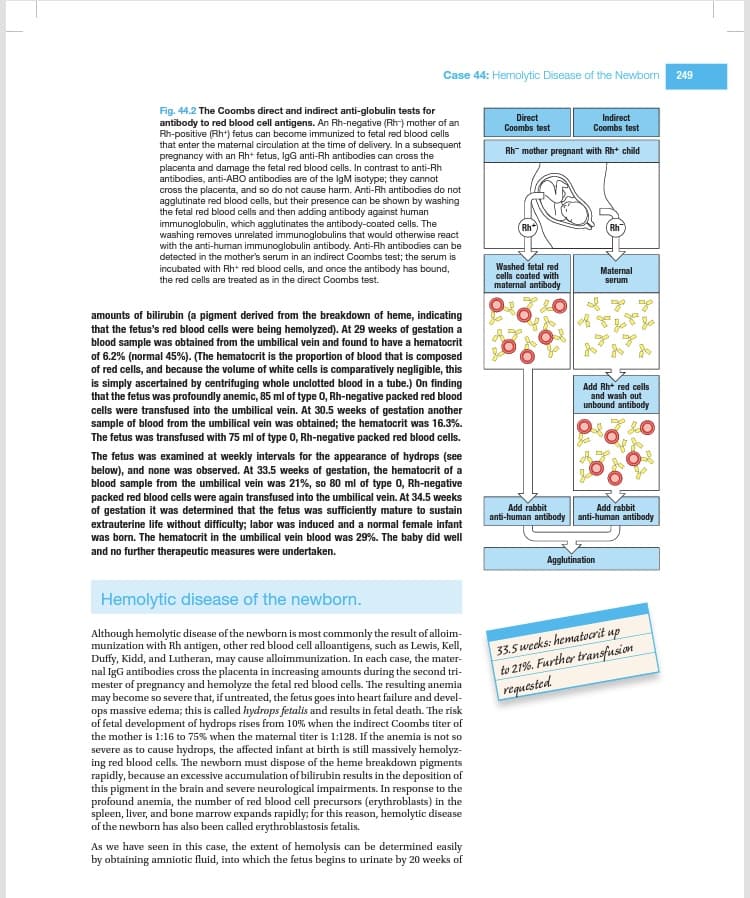
The Rh antigenic determinants are spaced very far apart on the red cell surface. As
a consequence, IgG antibodies against the Rh antigen do not fix complement and
therefore do not hemolyze red blood cells in vitro. For reasons that are less well
understood, IgG antibodies against the Rh antigen do not agglutinate Rh-positive
red blood cells. Because of this it was very difficult to detect Rh antibodies until
Robin Coombs at the University of Cambridge devised a solution to the prob-
lem by developing antibodies against human immunoglobulin. He showed that
Rh-positive red blood cells coated with IgG anti-Rh antibodies could be taken from
a fetus and agglutinated by antibodies against IgG. Furthermore, he showed that
when the serum of an alloimmunized woman was incubated with Rh-positive red
blood cells, these red blood cells could then be agglutinated by antibody against
IgG (Fig. 44.2). The former is called the direct Coombs test and the latter the indi-
rect Coombs test. This application of immunology to a vexing clinical problem led
ultimately to treatment and prevention of the problem.
The case of Cynthia Waymarsh: a fetus in
immunological distress.
Mrs Waymarsh was 31 years old when she became pregnant for the third time. She
was known to have blood group A, Rh-negative red cells. Her husband was also
type A but Rh-positive. Their first-born child, a male, was healthy. During her second
pregnancy Mrs Waymarsh was noted to have an indirect Coombs titer at a 1:16 dilu-
tion of her serum. The fetus was followed closely, and the delivery of a healthy baby
girl was induced at 36 weeks of gestation.
Five years later, Mrs Waymarsh became pregnant again. At 14 weeks of gestation
her indirect Coombs titer was 1:8, and at 18 weeks it was 1:16. Amniotic fluid was
obtained at 22, 24, 27, and 29 weeks of gestation and was found to have increasing
Transcribed Image Text:Case 44: Hemolytic Disease of the Newborn
Fig. 44.2 The Coombs direct and indirect anti-globulin tests for
antibody to red blood cell antigens. An Rh-negative (Rh-) mother of an
Rh-positive (Rh+) fetus can become immunized to fetal red blood cells
that enter the maternal circulation at the time of delivery. In a subsequent
pregnancy with an Rh+ fetus, IgG anti-Rh antibodies can cross the
placenta and damage the fetal red blood cells. In contrast to anti-Rh
antibodies, anti-ABO antibodies are of the IgM isotype; they cannot
cross the placenta, and so do not cause harm. Anti-Rh antibodies do not
agglutinate red blood cells, but their presence can be shown by washing
the fetal red blood cells and then adding antibody against human
immunoglobulin, which agglutinates the antibody-coated cells. The
washing removes unrelated immunoglobulins that would otherwise react
with the anti-human immunoglobulin antibody. Anti-Rh antibodies can be
detected in the mother's serum in an indirect Coombs test; the serum is
incubated with Rh+ red blood cells, and once the antibody has bound,
the red cells are treated as in the direct Coombs test.
amounts of bilirubin (a pigment derived from the breakdown of heme, indicating
that the fetus's red blood cells were being hemolyzed). At 29 weeks of gestation a
blood sample was obtained from the umbilical vein and found to have a hematocrit
of 6.2% (normal 45%). (The hematocrit is the proportion of blood that is composed
of red cells, and because the volume of white cells is comparatively negligible, this
is simply ascertained by centrifuging whole unclotted blood in a tube.) On finding
that the fetus was profoundly anemic, 85 ml of type 0, Rh-negative packed red blood
cells were transfused into the umbilical vein. At 30.5 weeks of gestation another
sample of blood from the umbilical vein was obtained; the hematocrit was 16.3%.
The etus was transfused with 75 ml of type 0, Rh-negative packed red blood cells.
The fetus was examined at weekly intervals for the appearance of hydrops (see
below), and none was observed. At 33.5 weeks of gestation, the hematocrit of a
blood sample from the umbilical vein was 21%, so 80 ml of type 0, Rh-negative
packed red blood cells were again transfused into the umbilical vein. At 34.5 weeks
of gestation it was determined that the fetus was sufficiently mature to sustain
extrauterine life without difficulty; labor was induced and a normal female infant
was born. The hematocrit in the umbilical vein blood was 29%. The baby did well
and no further therapeutic measures were undertaken.
Hemolytic disease of the newborn.
Although hemolytic disease of the newborn is most commonly the result of alloim-
munization with Rh antigen, other red blood cell alloantigens, such as Lewis, Kell,
Duffy, Kidd, and Lutheran, may cause alloimmunization. In each case, the mater-
nal IgG antibodies cross the placenta in increasing amounts during the second tri-
mester of pregnancy and hemolyze the fetal red blood cells. The resulting anemia
may become so severe that, if untreated, the fetus goes into heart failure and devel-
ops massive edema; this is called hydrops fetalis and results in fetal death. The risk
of fetal development of hydrops rises from 10% when the indirect Coombs titer of
the mother is 1:16 to 75% when the maternal titer is 1:128. If the anemia is not so
severe as to cause hydrops, the affected infant at birth is still massively hemolyz-
ing red blood cells. The newborn must dispose of the heme breakdown pigments
rapidly, because an excessive accumulation of bilirubin results in the deposition of
this pigment in the brain and severe neurological impairments. In response to the
profound anemia, the number of red blood cell precursors (erythroblasts) in the
spleen, liver, and bone marrow expands rapidly; for this reason, hemolytic disease
of the newborn has also been called erythroblastosis fetalis.
As we have seen in this case, the extent of hemolysis can be determined easily
by obtaining amniotic fluid, into which the fetus begins to urinate by 20 weeks of
Direct
Coombs test
Indirect
Coombs test
Rh- mother pregnant with Rh+ child
(Rh*
Washed fetal red
cells coated with
maternal antibody
Add rabbit
anti-human antibody
Rh
Maternal
serum
Add Rh+ red cells
and wash out
unbound antibody
Agglutination
Add rabbit
anti-human antibody
33.5 weeks: hematocrit up
to 21%. Further transfusion
requested.
249
Expert Solution
This question has been solved!
Explore an expertly crafted, step-by-step solution for a thorough understanding of key concepts.
This is a popular solution!
Trending now
This is a popular solution!
Step by step
Solved in 3 steps
Follow-up Questions
Read through expert solutions to related follow-up questions below.
Follow-up Question
Why were RH-negative red blood cells used for the intrauterine transfusion?
Solution
Knowledge Booster
Learn more about
Need a deep-dive on the concept behind this application? Look no further. Learn more about this topic, biology and related others by exploring similar questions and additional content below.Recommended textbooks for you

Anatomy & Physiology
Biology
ISBN:
9781938168130
Author:
Kelly A. Young, James A. Wise, Peter DeSaix, Dean H. Kruse, Brandon Poe, Eddie Johnson, Jody E. Johnson, Oksana Korol, J. Gordon Betts, Mark Womble
Publisher:
OpenStax College

Anatomy & Physiology
Biology
ISBN:
9781938168130
Author:
Kelly A. Young, James A. Wise, Peter DeSaix, Dean H. Kruse, Brandon Poe, Eddie Johnson, Jody E. Johnson, Oksana Korol, J. Gordon Betts, Mark Womble
Publisher:
OpenStax College