Surgical Tech For Surgical Tech Pos Care
5th Edition
ISBN:9781337648868
Author:Association
Publisher:Association
Chapter24: Neurosurgery
Section: Chapter Questions
Problem 24.2CS
Related questions
Question
3. List and briefly discuss the other types of bone and joint disorders besides rheumatoid arthritis.
4. Following a review of the laboratory tests, serum ALT and AST tests were performed. What is the reasoning
behind this? What medications does the patient currently take that necessitate this monitoring?
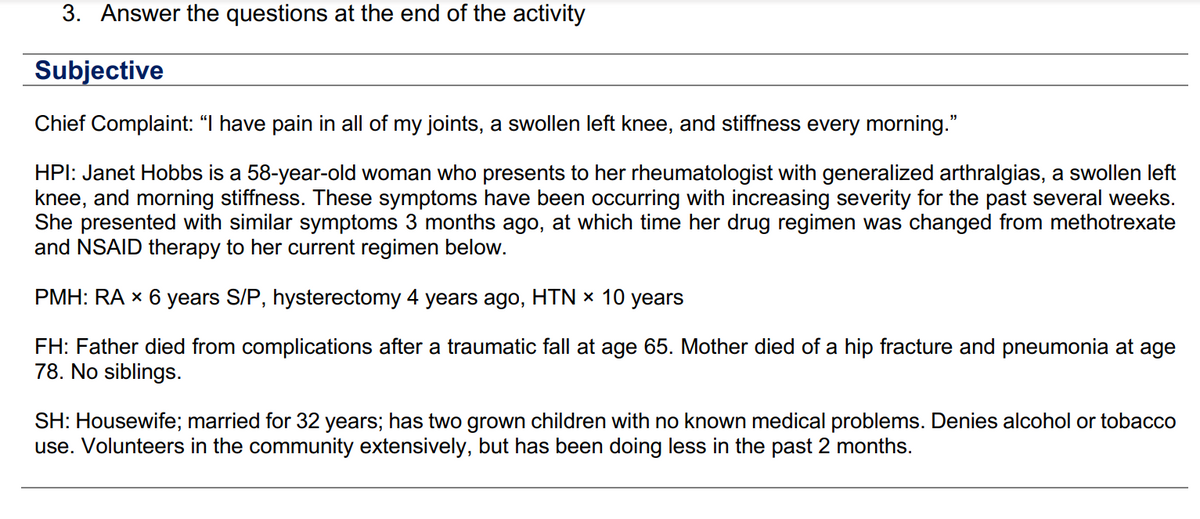
Transcribed Image Text:3. Answer the questions at the end of the activity
Subjective
Chief Complaint: “I have pain in all of my joints, a swollen left knee, and stiffness every morning."
HPI: Janet Hobbs is a 58-year-old woman who presents to her rheumatologist with generalized arthralgias, a swollen left
knee, and morning stiffness. These symptoms have been occurring with increasing severity for the past several weeks.
She presented with similar symptoms 3 months ago, at which time her drug regimen was changed from methotrexate
and NSAID therapy to her current regimen below.
PMH: RA × 6 years S/P, hysterectomy 4 years ago, HTN × 10 years
FH: Father died from complications after a traumatic fall at age 65. Mother died of a hip fracture and pneumonia at age
78. No siblings.
SH: Housewife; married for 32 years; has two grown children with no known medical problems. Denies alcohol or tobacco
use. Volunteers in the community extensively, but has been doing less in the past 2 months.
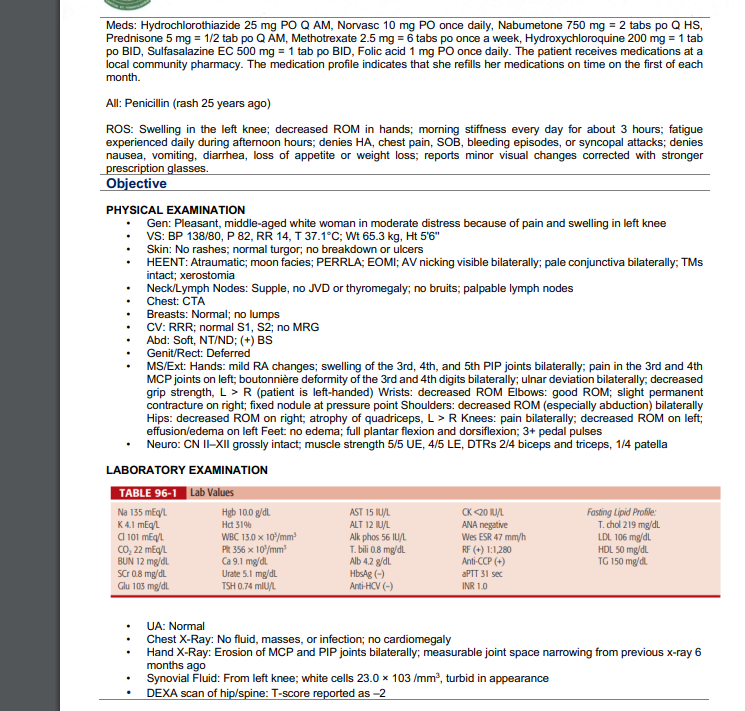
Transcribed Image Text:Meds: Hydrochlorothiazide 25 mg PO Q AM, Norvasc 10 mg PO once daily, Nabumetone 750 mg = 2 tabs po Q HS,
Prednisone 5 mg = 1/2 tab po Q AM, Methotrexate 2.5 mg = 6 tabs po once a week, Hydroxychloroquine 200 mg = 1 tab
po BID, Sulfasalazine EC 500 mg = 1 tab po BID, Folic acid 1 mg PO once daily. The patient receives medications at a
local community pharmacy. The medication profile indicates that she refills her medications on time on the first of each
month.
All: Penicillin (rash 25 years ago)
ROS: Swelling in the left knee; decreased ROM in hands; morning stiffness every day for about 3 hours; fatigue
experienced daily during afternoon hours; denies HA, chest pain, SOB, bleeding episodes, or syncopal attacks; denies
nausea, vomiting, diarrhea, loss of appetite or weight loss; reports minor visual changes corrected with stronger
prescription glasses.
Objective
PHYSICAL EXAMINATION
Gen: Pleasant, middle-aged white woman in moderate distress because of pain and swelling in left knee
VS: BP 138/80, P 82, RR 14, T 37.1°C; Wt 65.3 kg, Ht 5'6"
.
.
Skin: No rashes; normal turgor; no breakdown or ulcers
HEENT: Atraumatic; moon facies; PERRLA; EOMI; AV nicking visible bilaterally; pale conjunctiva bilaterally; TMs
intact; xerostomia
.
Neck/Lymph Nodes: Supple, no JVD or thyromegaly; no bruits; palpable lymph nodes
Chest: CTA
Breasts: Normal; no lumps
CV: RRR; normal S1, S2; no MRG
Abd: Soft, NT/ND; (+) BS
Genit/Rect: Deferred
LABORATORY EXAMINATION
TABLE 96-1 Lab Values
Na 135 mEq/L
K4.1 mEq/L
Cl101 mEq/L
CO₂ 22 mEq/L
BUN 12 mg/dL
SCr 0.8 mg/dL
Glu 103 mg/dL
MS/Ext: Hands: mild RA changes; swelling of the 3rd, 4th, and 5th PIP joints bilaterally; pain in the 3rd and 4th
MCP joints on left; boutonnière deformity of the 3rd and 4th digits bilaterally; ulnar deviation bilaterally, decreased
grip strength, L > R (patient is left-handed) Wrists: decreased ROM Elbows: good ROM; slight permanent
contracture on right; fixed nodule at pressure point Shoulders: decreased ROM (especially abduction) bilaterally
Hips: decreased ROM on right; atrophy of quadriceps, L > R Knees: pain bilaterally; decreased ROM on left;
effusion/edema on left Feet: no edema; full plantar flexion and dorsiflexion; 3+ pedal pulses
Neuro: CN II-XII grossly intact; muscle strength 5/5 UE, 4/5 LE, DTRS 2/4 biceps and triceps, 1/4 patella
Hgb 10.0 g/dl
Hct 31%
WBC 13.0 x 10/mm³
Plt 356 x 10³/mm³
Ca 9.1 mg/dl
Urate 5.1 mg/dL
TSH 0.74 mIU/L
AST 15 IU/L
ALT 12 IU/L
Alk phos 56 IU/L
T.bili 0.8 mg/dL
Alb 4.2 g/dL
HbsAg (-)
Anti-HCV (-)
CK <20 IU/L
ANA negative
Wes ESR 47 mm/h
RF (+) 1:1,280
Anti-CCP (+)
aPTT 31 sec
INR 1.0
Fasting Lipid Profile:
T. chol 219 mg/dL
LDL 106 mg/dl
HDL 50 mg/dL
TG 150 mg/dl.
UA: Normal
Chest X-Ray: No fluid, masses, or infection; no cardiomegaly
Hand X-Ray: Erosion of MCP and PIP joints bilaterally; measurable joint space narrowing from previous x-ray 6
months ago
Synovial Fluid: From left knee; white cells 23.0 x 103 /mm³, turbid in appearance
DEXA scan of hip/spine: T-score reported as -2
Expert Solution
This question has been solved!
Explore an expertly crafted, step-by-step solution for a thorough understanding of key concepts.
Step by step
Solved in 3 steps
Recommended textbooks for you

Surgical Tech For Surgical Tech Pos Care
Health & Nutrition
ISBN:
9781337648868
Author:
Association
Publisher:
Cengage


Comprehensive Medical Assisting: Administrative a…
Nursing
ISBN:
9781305964792
Author:
Wilburta Q. Lindh, Carol D. Tamparo, Barbara M. Dahl, Julie Morris, Cindy Correa
Publisher:
Cengage Learning

Surgical Tech For Surgical Tech Pos Care
Health & Nutrition
ISBN:
9781337648868
Author:
Association
Publisher:
Cengage


Comprehensive Medical Assisting: Administrative a…
Nursing
ISBN:
9781305964792
Author:
Wilburta Q. Lindh, Carol D. Tamparo, Barbara M. Dahl, Julie Morris, Cindy Correa
Publisher:
Cengage Learning

Essentials of Pharmacology for Health Professions
Nursing
ISBN:
9781305441620
Author:
WOODROW
Publisher:
Cengage

Basic Clinical Lab Competencies for Respiratory C…
Nursing
ISBN:
9781285244662
Author:
White
Publisher:
Cengage
