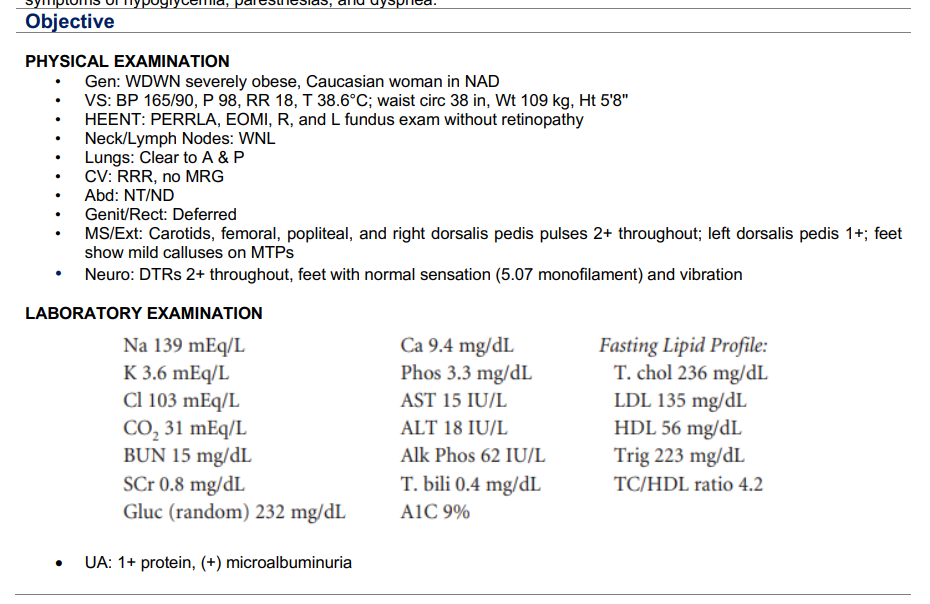
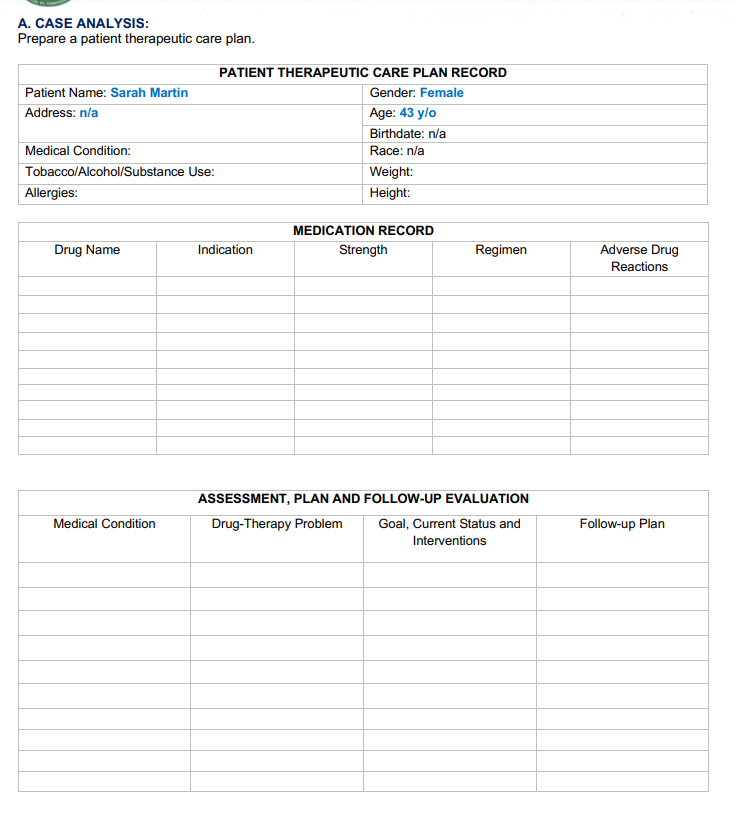
Subjective Chief Complaint: “I was recently diagnosed with possible diabetes and would like to have my blood sugar tested. I think that my blood sugar is running low because I have a terrible headache.” HPI: Sarah Martin is a 43-year-old woman who comes to the pharmacy for a diabetes education class taught by the pharmacist. She would like for the pharmacist to check her blood sugar before the class begins. She was diagnosed with diabetes mellitus Type 2 about 6 months ago. She has been attempting to control her disease with diet and exercise but has had no success. Her physician has recently started her on glyburide 5 mg. She has gained 15 lb. over the past year. She monitors her blood sugar once a day, per her physician, with a range of 215–260 mg/dL. Her fasting blood sugars average 170 mg/dL. PMH: Type 2 DM × 6 months, HTN × 15 years, bipolar disorder × 25 years, Dyslipidemia × 10 years, Morbid obesity × 15 years FH: Father has a history of HTN and bipolar disorder. The mother has a history of dyslipidemia. Brother has DM secondary to alcoholism. SH: Has been married for 21 years. She has two children who are teenagers. She works in a floral shop making deliveries. Denies any use of tobacco products but does drink alcohol occasionally (five beers/wine per week). Meds: Glyburide 5 mg po BID, Lisinopril 20 mg po once daily, Zyprexa 5 mg po Q HS, Carbamazepine 200 mg po TID, Lorazepam 1 mg po TID PRN, Fluoxetine 20 mg po Q AM, EC ASA 81 mg po once daily, Pravastatin 40 mg po once daily All: Morphine—hives ROS: Complaints of nocturia, polyuria, and polydipsia on a daily basis. Denies nausea, constipation, diarrhea, signs or symptoms of hypoglycemia, paresthesias, and dyspnea. Kindly answer the case study therapeutic plan. TYSM
Subjective
Chief Complaint: “I was recently diagnosed with possible diabetes and would like to have my blood sugar tested. I think that my blood sugar is running low because I have a terrible headache.”
HPI: Sarah Martin is a 43-year-old woman who comes to the pharmacy for a diabetes education class taught by the
pharmacist. She would like for the pharmacist to check her blood sugar before the class begins. She was diagnosed with diabetes mellitus Type 2 about 6 months ago. She has been attempting to control her disease with diet and exercise but has had no success. Her physician has recently started her on glyburide 5 mg. She has gained 15 lb. over the past year. She monitors her blood sugar once a day, per her physician, with a range of 215–260 mg/dL. Her fasting blood sugars average 170 mg/dL.
PMH: Type 2 DM × 6 months, HTN × 15 years, bipolar disorder × 25 years, Dyslipidemia × 10 years, Morbid obesity × 15 years
FH: Father has a history of HTN and bipolar disorder. The mother has a history of dyslipidemia. Brother has DM secondary to alcoholism.
SH: Has been married for 21 years. She has two children who are teenagers. She works in a floral shop making deliveries. Denies any use of tobacco products but does drink alcohol occasionally (five beers/wine per week).
Meds: Glyburide 5 mg po BID, Lisinopril 20 mg po once daily, Zyprexa 5 mg po Q HS, Carbamazepine 200 mg po TID, Lorazepam 1 mg po TID PRN, Fluoxetine 20 mg po Q AM, EC ASA 81 mg po once daily, Pravastatin 40 mg po once daily
All: Morphine—hives
ROS: Complaints of nocturia, polyuria, and polydipsia on a daily basis. Denies nausea, constipation, diarrhea, signs or symptoms of hypoglycemia, paresthesias, and dyspnea.
Kindly answer the case study therapeutic plan. TYSM
Trending now
This is a popular solution!
Step by step
Solved in 2 steps