A. M.tuberculosis (Mtb) takes about 12h to 18h to do a cell division. This partially explains why it takes so long to grow the bacteria for diagnosis (4-6 weeks). How can this impact treatment? Be precise. B. Which group of patients will be the most challenging to treat? Explain why you chose that group? Be precise.
A. M.tuberculosis (Mtb) takes about 12h to 18h to do a cell division. This partially explains why it takes so long to grow the bacteria for diagnosis (4-6 weeks). How can this impact treatment? Be precise. B. Which group of patients will be the most challenging to treat? Explain why you chose that group? Be precise.
Comprehensive Medical Assisting: Administrative and Clinical Competencies (MindTap Course List)
6th Edition
ISBN:9781305964792
Author:Wilburta Q. Lindh, Carol D. Tamparo, Barbara M. Dahl, Julie Morris, Cindy Correa
Publisher:Wilburta Q. Lindh, Carol D. Tamparo, Barbara M. Dahl, Julie Morris, Cindy Correa
Chapter21: Infection Control And Medical Asepsis
Section: Chapter Questions
Problem 21.1CS
Related questions
Question
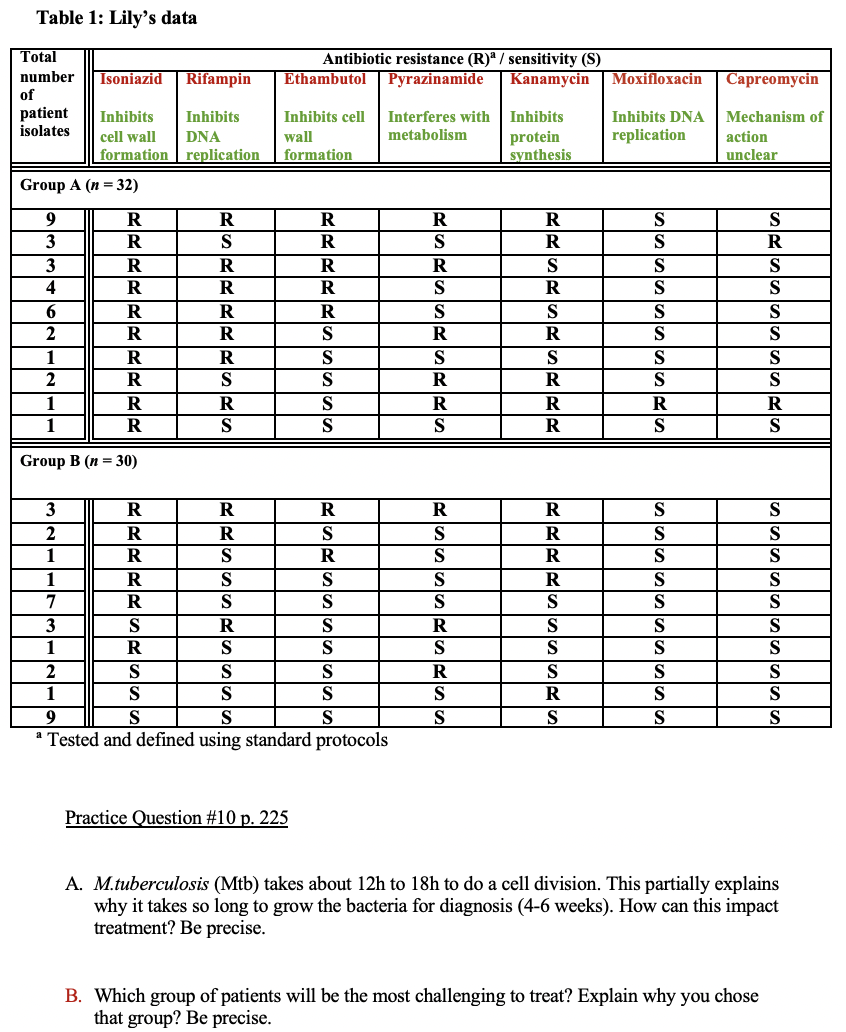
Transcribed Image Text:Table 1: Lily's data
Total
Antibiotic resistance (R) / sensitivity (S)
Pyrazinamide
number
Isoniazid
Rifampin
Ethambutol
Kanamycin
МоxiПlохасin
Capreomycin
of
patient
isolates
Inhibits
Inhibits
Inhibits cell
Interferes with
Inhibits
Inhibits DNA
Mechanism of
DNA
metabolism
replication
protein
synthesis
cell wall
wall
action
formation replication
formation
unclear
Group A (n = 32)
9
R
R
R
S
S
3
R
S
R
S
S
R
3
R
S
S
S
4
R
R
S
R
S
S
R
R
R
S
S
S
S
2
R
R
R
S
1
R
S
S
S
S
S
2
R
R
S
1
R
R
S
R
R
R
1
R
R
S
Group B (n = 30)
3
R
R
S
2
R
S
S
R
S
S
1
R
S
R
S
R
S
S
1
R
S
S
S
R
S
S
7
R
S
S
S
3
S
R
S
R
S
S
S
1
R
S
S
S
S
2
S
S
R
S
S
S
1
S
S
R
S
S
a Tested and defined using standard protocols
9
S
S
S
S
Practice Question #10 p. 225
A. M.tuberculosis (Mtb) takes about 12h to 18h to do a cell division. This partially explains
why it takes so long to grow the bacteria for diagnosis (4-6 weeks). How can this impact
treatment? Be precise.
B. Which group of patients will be the most challenging to treat? Explain why you chose
that group? Be precise.
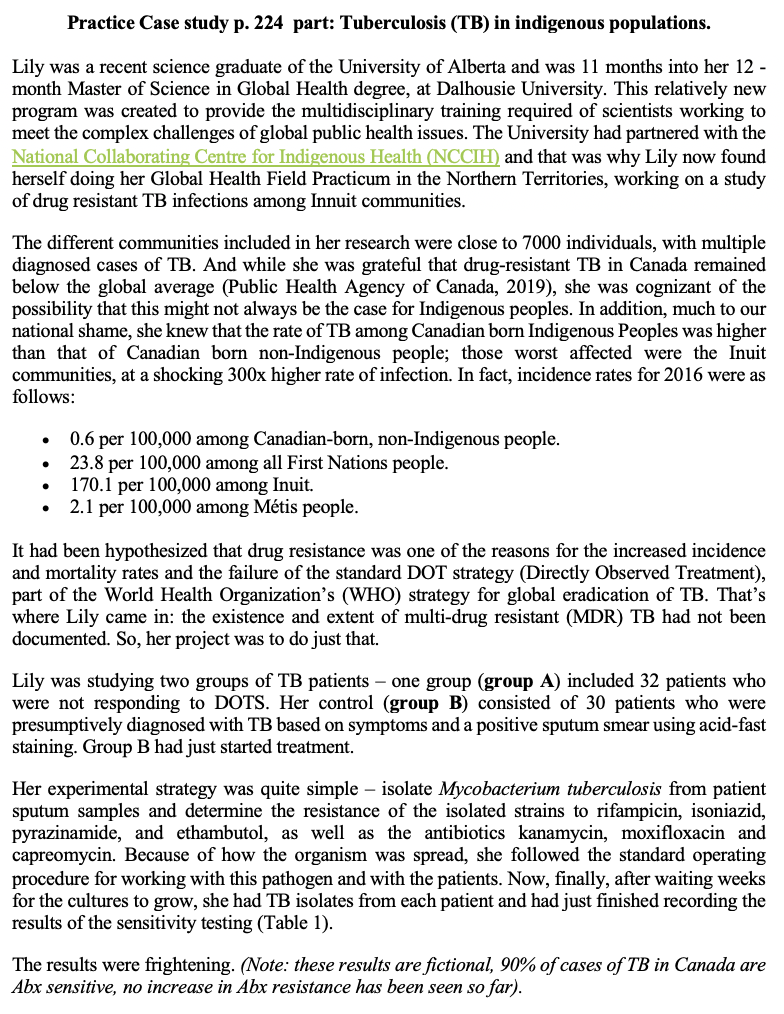
Transcribed Image Text:Practice Case study p. 224 part: Tuberculosis (TB) in indigenous populations.
Lily was a recent science graduate of the University of Alberta and was 11 months into her 12 -
month Master of Science in Global Health degree, at Dalhousie University. This relatively new
program was created to provide the multidisciplinary training required of scientists working to
meet the complex challenges of global public health issues. The University had partnered with the
National Collaborating Centre for Indigenous Health (NCCIH) and that was why Lily now found
herself doing her Global Health Field Practicum in the Northern Territories, working on a study
of drug resistant TB infections among Innuit communities.
The different communities included in her research were close to 7000 individuals, with multiple
diagnosed cases of TB. And while she was grateful that drug-resistant TB in Canada remained
below the global average (Public Health Agency of Canada, 2019), she was cognizant of the
possibility that this might not always be the case for Indigenous peoples. In addition, much to our
national shame, she knew that the rate of TB among Canadian born Indigenous Peoples was higher
than that of Canadian born non-Indigenous people; those worst affected were the Inuit
communities, at a shocking 300x higher rate of infection. In fact, incidence rates for 2016 were as
follows:
0.6 per 100,000 among Canadian-born, non-Indigenous people.
per 100,000 among all First Nations people.
170.1 per 100,000 among Inuit.
2.1 per 100,000 among Métis people.
It had been hypothesized that drug resistance was one of the reasons for the increased incidence
and mortality rates and the failure of the standard DOT strategy (Directly Observed Treatment),
part of the World Health Organization's (WHO) strategy for global eradication of TB. That's
where Lily came in: the existence and extent of multi-drug resistant (MDR) TB had not been
documented. So, her project was to do just that.
Lily was studying two groups of TB patients – one group (group A) included 32 patients who
were not responding to DOTS. Her control (group B) consisted of 30 patients who were
presumptively diagnosed with TB based on symptoms and a positive sputum smear using acid-fast
staining. Group B had just started treatment.
Her experimental strategy was quite simple – isolate Mycobacterium tuberculosis from patient
sputum samples and determine the resistance of the isolated strains to rifampicin, isoniazid,
pyrazinamide, and ethambutol, as well as the antibiotics kanamycin, moxifloxacin and
capreomycin. Because of how the organism was spread, she followed the standard operating
procedure for working with this pathogen and with the patients. Now, finally, after waiting weeks
for the cultures to grow, she had TB isolates from each patient and had just finished recording the
results of the sensitivity testing (Table 1).
The results were frightening. (Note: these results are fictional, 90% of cases of TB in Canada are
Abx sensitive, no increase in Abx resistance has been seen so far).
Expert Solution
This question has been solved!
Explore an expertly crafted, step-by-step solution for a thorough understanding of key concepts.
Step by step
Solved in 2 steps
Knowledge Booster
Learn more about
Need a deep-dive on the concept behind this application? Look no further. Learn more about this topic, biology and related others by exploring similar questions and additional content below.Recommended textbooks for you
Comprehensive Medical Assisting: Administrative a…
Nursing
ISBN:
9781305964792
Author:
Wilburta Q. Lindh, Carol D. Tamparo, Barbara M. Dahl, Julie Morris, Cindy Correa
Publisher:
Cengage Learning

Comprehensive Medical Assisting: Administrative a…
Nursing
ISBN:
9781305964792
Author:
Wilburta Q. Lindh, Carol D. Tamparo, Barbara M. Dahl, Julie Morris, Cindy Correa
Publisher:
Cengage Learning
